Science / Inflammatory Bowel Disease
Science / Inflammatory Bowel Disease
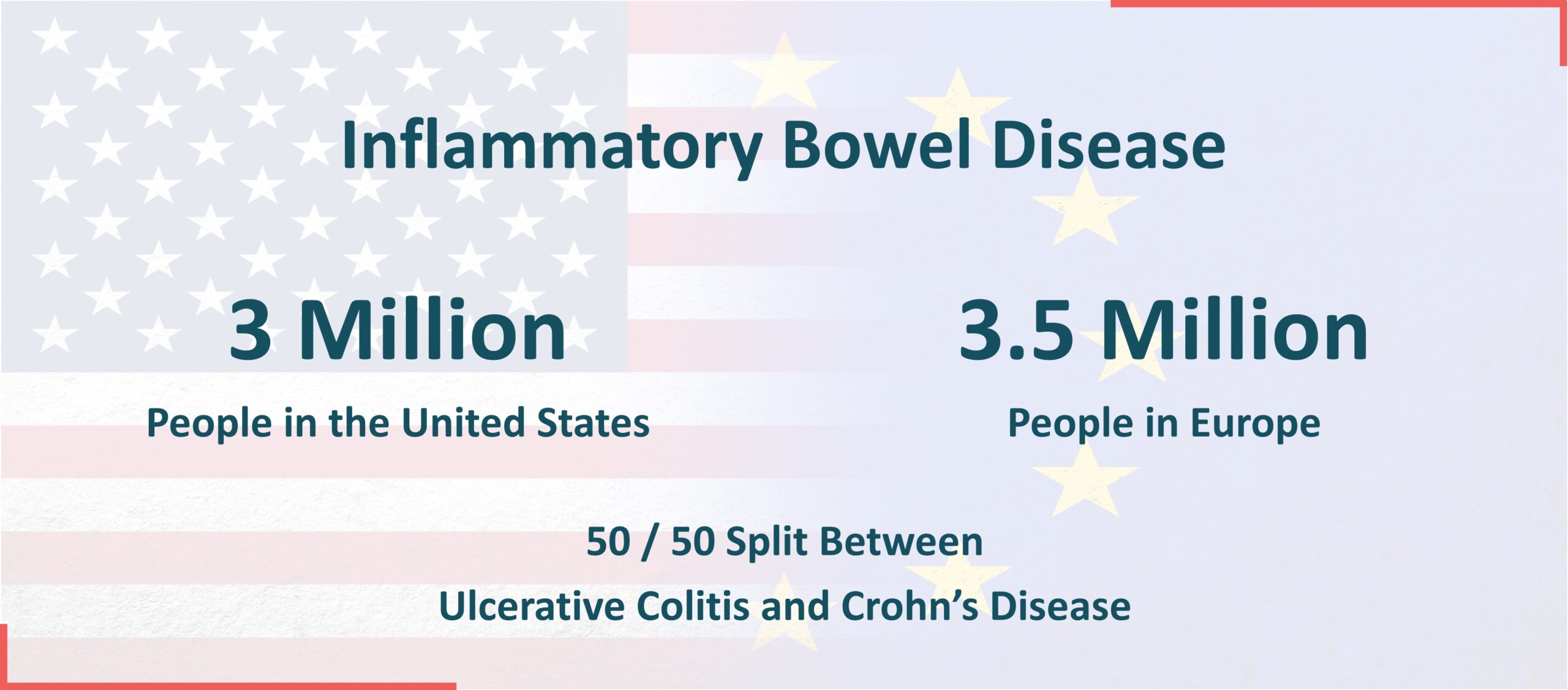
Inflammatory Bowel Disease (IBD)
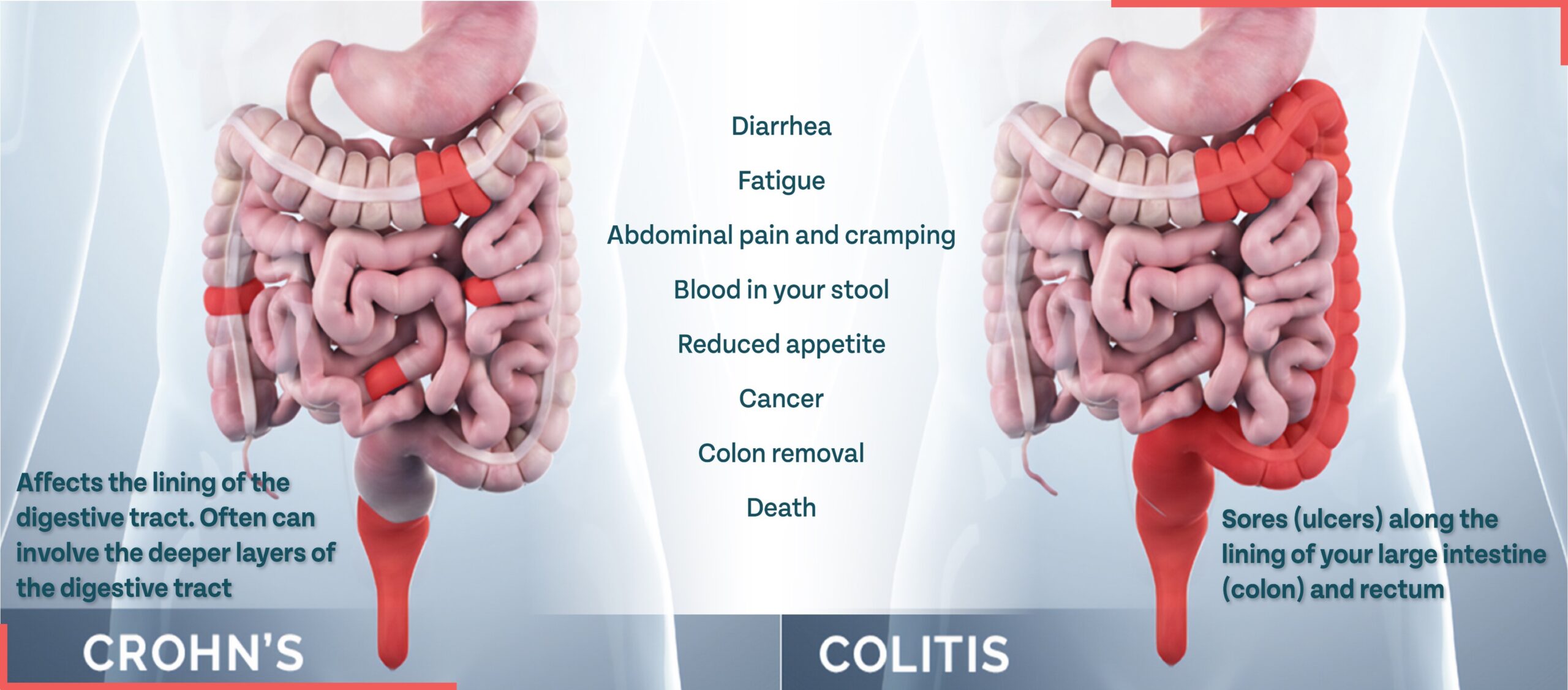
Inflammatory Bowel Disease (IBD) is a chronic medical condition characterized by inflammation of the digestive tract. It primarily includes two main types: Crohn’s disease and ulcerative colitis. While the cause of IBD is unknown, it can lead to a range of health risks, including nutritional deficiencies, infections, inflammation, heightened cancer risk, and potential complications like strictures and abscesses.
Currently available injectable biologic therapies are lacking and on average, only achieve a clinical remission rate of less than 20%. We believe there is a significant need for innovation and believe our precision delivery, oral PDE4 technology has the potential to address these deficiencies in the treatment of IBD.
Ulcerative Colitis and Crohn’s Disease Affect Different Areas of the Intestine but Can Both Impact Quality of Life
Our Innovative Approach to the Treatment of IBD
Precision Delivery for Patient-Tailored Therapies: Targeting PDE4
Our Precision Delivery Platform uses the phosphodiesterase-4 (PDE4) enzyme as its first therapeutic target. PDE4 is highly expressed in immune and proinflammatory cells. The inhibition of PDE4 prevents transcription factors, such as NF-κB, from inducing the expression of various proinflammatory mediators involved in IBD, such as TNF-α and various interleukins.

Gut Restricted Approach
Following oral administration, our prodrug candidates are first inactive, poorly absorbed and remain restricted to the gut. This prevents systemic exposure of their active form allowing for safer therapies. Once activated by the gut microbiota at desired location, high concentration of the active drug is achieved locally at the site of inflammation in the GI tract.

Pro-Drug Provides Potential for Improved Safety Over Approved Therapies
- Bioactivation at the site of inflammation
- Low absorption in the upper GI tract
- No premature prodrug bioactivation in the upper GI
- Limited systemic exposure
Technology
Active digestive enzymes are normally found in the small intestine where they digest food. If these enzymes become active outside the intestines, they start “digesting” healthy tissue, a process called autodigestion.
Autodigestion may lead to complications such as adhesions (scar tissue that binds organs and tissues that are not usually connected), proteolytic cleavage of cell membrane receptors leading to impaired cellular function, and chronic inflammation.
Our lead asset, LB1148, is a broad-spectrum serine protease inhibitor which acts to neutralize digestive enzymes, potentially reducing intestinal damage. LB1148 is being investigated in a Phase 2 study to evaluate its effects on intra-abdominal adhesions and return of gastrointestinal function in subjects undergoing elective bowel resection.
Our Innovation Story
Disruption in the integrity of the gastrointestinal barrier can have a cascade effect on GI health, as well as lead to the onset of oncologic, metabolic, cardiovascular, and neurological diseases. Our innovative track record has empowered us to change the future of GI surgery and treat the multitude of serious diseases caused by disruption of intestinal integrity.